Tb Test PDF Form
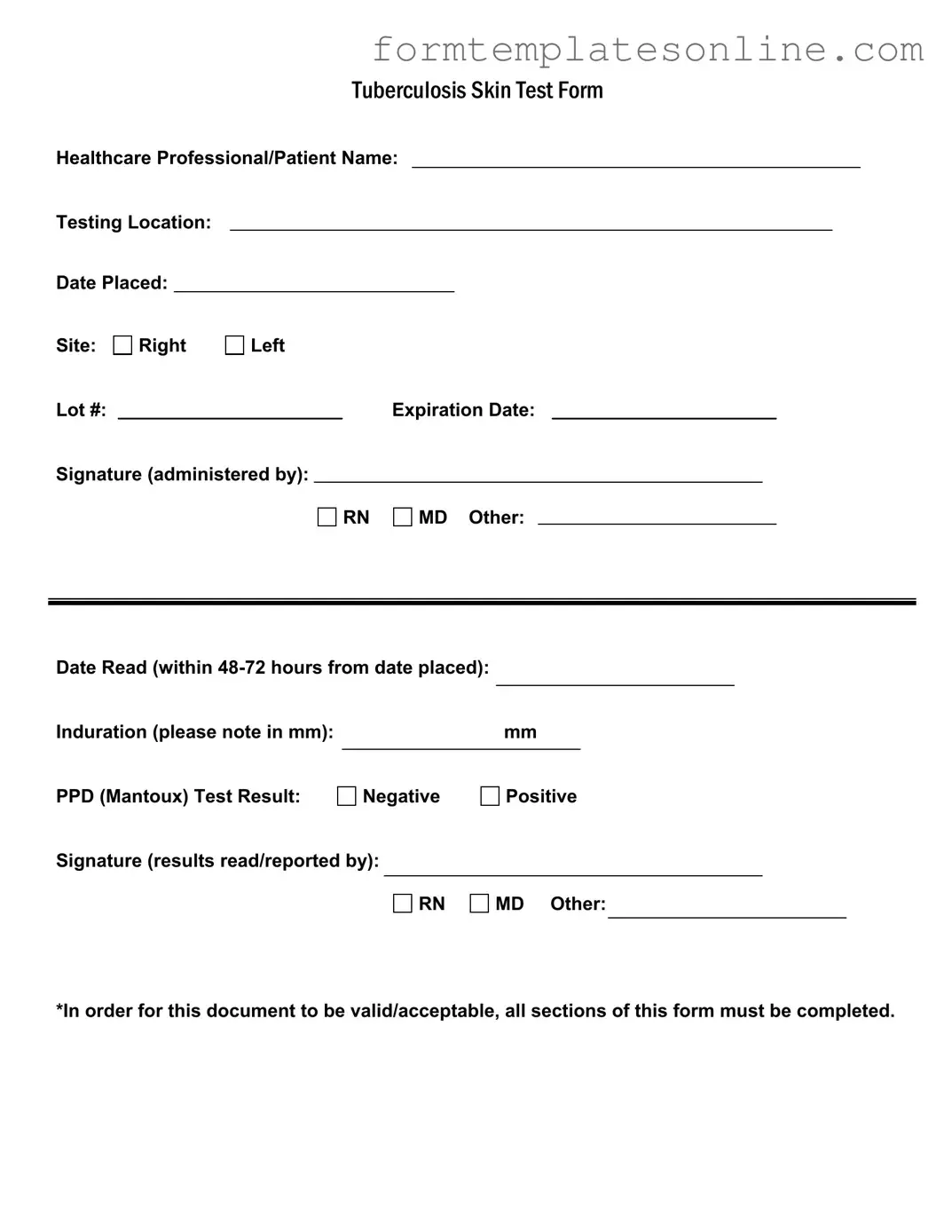
The Tuberculosis Skin Test (Tb Test) form serves as a critical tool in the screening and diagnosis of tuberculosis, a serious infectious disease. This form captures essential information, including the healthcare professional's and patient's names, the testing location, and the date the test was placed. It also specifies the site of the test—either the right or left arm—along with details such as the lot number and expiration date of the testing material. The signature of the administering professional, whether a registered nurse (RN), medical doctor (MD), or other qualified personnel, is required to validate the procedure. Following the test, results must be read within 48 to 72 hours, with the induration measured in millimeters noted on the form. The final outcome of the PPD (Mantoux) test is clearly indicated as either negative or positive, alongside the signature of the individual who reported the results. It is crucial that all sections of the form are completed for it to be considered valid and acceptable, ensuring accurate documentation and follow-up care for the patient.
Common mistakes
-
Incomplete Information: Many individuals forget to fill out all sections of the form. Each field, including the healthcare professional's name, testing location, and date placed, is essential for proper documentation.
-
Incorrect Measurement: When noting the induration in millimeters, some people either mismeasure or fail to record the result altogether. Accurate measurement is crucial for determining the test outcome.
-
Missing Signatures: It's common to overlook the requirement for signatures. Both the healthcare professional administering the test and the one reading the results must sign the form to validate it.
-
Ignoring Expiration Dates: Individuals sometimes forget to check the expiration date of the PPD solution. Using expired materials can lead to inaccurate results, rendering the test invalid.
Example - Tb Test Form
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.
More About Tb Test
What is the purpose of the TB Test form?
The TB Test form is used to document the administration and results of the Tuberculosis (TB) skin test, commonly known as the PPD or Mantoux test. This form ensures that healthcare professionals have a record of the test details, including the testing location, date placed, and the results, which are crucial for diagnosing TB infection.
Who needs to fill out the TB Test form?
The TB Test form must be completed by a healthcare professional who administers the test. Additionally, the patient’s information should be included to maintain accurate records. It is important for both parties to ensure that all necessary details are filled out correctly.
What information is required on the TB Test form?
Essential information includes the healthcare professional's name, the patient's name, the testing location, the date the test was placed, and the site of administration (right or left arm). The form also requires the lot number and expiration date of the test material, along with the signature of the administering professional.
How soon should the TB Test results be read?
The results of the TB test must be read within 48 to 72 hours after the test is placed. This timeframe is critical, as it allows healthcare professionals to accurately assess the induration (swelling) at the test site, which determines whether the result is positive or negative.
What does it mean if the TB Test result is positive?
A positive TB Test result indicates that the person has been exposed to the TB bacteria. It does not necessarily mean that the person has an active TB infection. Further evaluation, including a chest X-ray and possibly additional tests, may be required to determine if the person is infected and needs treatment.
What should be done if the TB Test result is negative?
A negative TB Test result generally suggests that the person has not been exposed to the TB bacteria. However, it is important to consider any potential risk factors, such as recent exposure or symptoms of TB. If there are concerns, consult a healthcare professional for further advice.
What happens if the TB Test form is incomplete?
If any section of the TB Test form is left incomplete, the document may be deemed invalid or unacceptable. It is crucial for both the healthcare professional and the patient to ensure that all required fields are filled out accurately before submission.
Who is responsible for reporting the results of the TB Test?
The healthcare professional who reads the results is responsible for reporting them. This individual must sign the form, indicating that they have reviewed the results and communicated them to the patient. Accurate reporting is essential for proper follow-up and treatment if necessary.
Can the TB Test form be used for employment or school requirements?
Yes, many employers and educational institutions require proof of a negative TB test for employment or enrollment. The completed TB Test form serves as official documentation of the test results and may be submitted as part of the application or onboarding process.
Key takeaways
Here are some key takeaways for filling out and using the TB Test form:
- Complete All Sections: Ensure every section of the form is filled out. Incomplete forms may not be accepted.
- Patient and Healthcare Professional Information: Clearly write the names of both the healthcare professional and the patient at the top of the form.
- Testing Location: Specify where the test is being conducted. This information is crucial for record-keeping.
- Date Placed: Record the exact date the test is administered. This is important for follow-up.
- Induration Measurement: Measure the induration in millimeters after 48-72 hours. This result is vital for determining the test outcome.
- Test Result: Clearly indicate whether the PPD (Mantoux) test result is negative or positive. This will guide further action.
- Signature Requirement: Both the administering professional and the individual reading the results must sign the form.
- Expiration Date: Check the expiration date of the lot number used for the test. Using expired materials can lead to inaccurate results.
- Documentation: Keep a copy of the completed form for your records. This can be important for future medical needs.
Form Attributes
| Fact Name | Description |
|---|---|
| Form Purpose | The Tuberculosis Skin Test Form is used to document the administration and results of the TB skin test, a common method for screening tuberculosis infection. |
| Completion Requirement | All sections of the form must be completed for it to be considered valid and acceptable. This includes patient information, testing details, and results. |
| Reading Window | The test must be read within 48 to 72 hours from the date it was placed to ensure accurate results. |
| Result Interpretation | The results are categorized as either negative or positive, based on the induration measured in millimeters at the test site. |
| State-Specific Laws | In California, for instance, the TB test form is governed by Title 17 of the California Code of Regulations, which outlines public health requirements for TB screening. |
Other PDF Forms
Miscellaneous Information - The form must be filled out accurately to avoid issues with the IRS during tax filing season.
For those seeking to manage their affairs effectively, the Florida General Power of Attorney form serves as a crucial tool that delegates authority to another individual. It is vital to familiarize yourself with the implications of this document to protect your interests in situations where you may be unable to make decisions on your own. You can learn more about this vital legal instrument through this helpful General Power of Attorney resource.
Blank 1099 Nec Form 2023 - A separate 1099-NEC should be filled out for each recipient paid during the tax year.
Florida Dh 680 Form Printable - This form is required by Florida law and must be completed for K-12 school admission.
Dos and Don'ts
When filling out the TB Test form, it’s important to ensure accuracy and completeness. Here are some guidelines to follow:
- Do fill in all required fields completely, including the healthcare professional's name, testing location, and dates.
- Do clearly indicate the induration measurement in millimeters, as this is crucial for interpreting the test results.
- Do ensure that the signature of the healthcare professional administering the test is included, along with their designation.
- Do double-check the expiration date of the PPD solution used, as expired solutions can lead to inaccurate results.
- Don't leave any sections blank, as incomplete forms may not be accepted.
- Don't use abbreviations or unclear handwriting; clarity is essential for proper interpretation.
- Don't forget to record the date the test was read, as this must be within 48-72 hours of placement.
- Don't neglect to document the test result accurately, whether negative or positive.