Annual Physical Examination PDF Form
The Annual Physical Examination form is a crucial document that plays a significant role in ensuring an individual's health is thoroughly assessed and monitored. This form is designed to gather essential information prior to a medical appointment, allowing healthcare providers to have a comprehensive understanding of a patient's medical history and current health status. Key sections of the form include personal details such as name, date of birth, and address, as well as critical health information like diagnoses, current medications, and allergies. Additionally, it prompts patients to provide details about their immunizations and any recent medical tests or screenings. The form also covers general physical examination metrics, including vital signs and evaluations of various body systems. It encourages a holistic approach by asking about lifestyle factors and any necessary recommendations for health maintenance. By completing this form accurately, individuals can help ensure that their healthcare providers are well-informed and can deliver the best possible care during their visit.
Common mistakes
-
Incomplete Personal Information: Failing to fill out all sections, such as name, address, or date of birth, can lead to confusion or delays in care.
-
Missing Medical History: Not providing a comprehensive medical history summary, including chronic health problems, can hinder accurate diagnosis and treatment.
-
Omitting Current Medications: Leaving out details about current medications, including dosage and frequency, may result in dangerous drug interactions.
-
Ignoring Allergies: Failing to list allergies or sensitivities can put individuals at risk during medical procedures or when prescribing new medications.
-
Inaccurate Immunization Records: Not updating or providing incorrect dates for immunizations can lead to unnecessary vaccinations or missed boosters.
-
Neglecting TB Screening Details: Omitting the dates and results of tuberculosis screenings can delay necessary follow-up actions.
-
Overlooking Past Hospitalizations: Not documenting previous hospitalizations or surgeries can prevent healthcare providers from understanding the full health picture.
-
Skipping Evaluation of Systems: Failing to answer questions about normal findings for various systems may lead to missed health issues.
-
Not Providing Additional Comments: Leaving the additional comments section blank can limit the physician's understanding of specific concerns or changes in health status.
Example - Annual Physical Examination Form
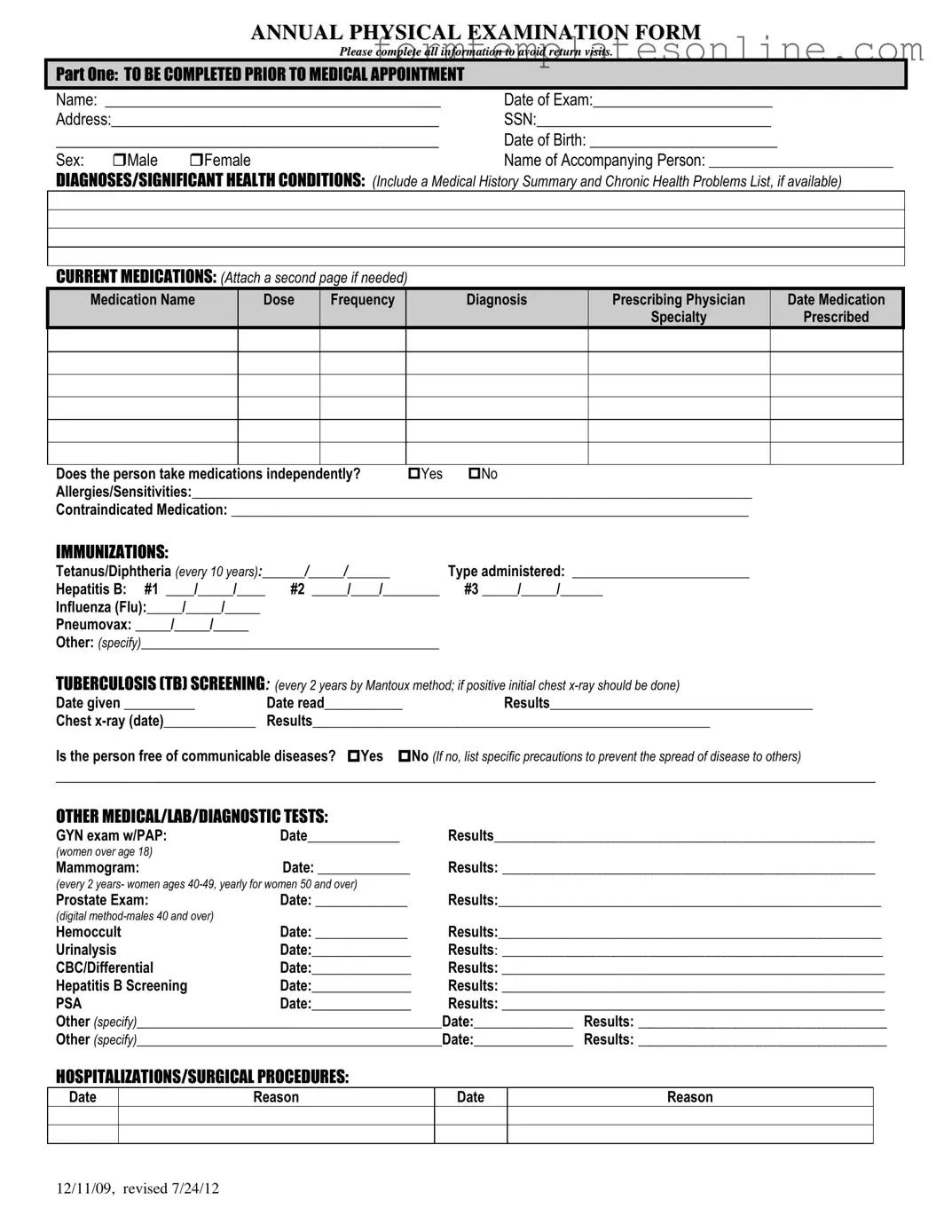
ANNUAL PHYSICAL EXAMINATION FORM
Please complete all information to avoid return visits.
PART ONE: TO BE COMPLETED PRIOR TO MEDICAL APPOINTMENT
Name: ___________________________________________ |
Date of Exam:_______________________ |
Address:__________________________________________ |
SSN:______________________________ |
_____________________________________________ |
Date of Birth: ________________________ |
||
Sex: |
Male |
Female |
Name of Accompanying Person: __________________________ |
DIAGNOSES/SIGNIFICANT HEALTH CONDITIONS: (Include a Medical History Summary and Chronic Health Problems List, if available)
CURRENT MEDICATIONS: (Attach a second page if needed)
Medication Name |
Dose |
Frequency |
Diagnosis |
Prescribing Physician |
Date Medication |
|
|
|
|
Specialty |
Prescribed |
Does the person take medications independently? |
Yes |
No |
Allergies/Sensitivities:_______________________________________________________________________________ |
||
Contraindicated Medication: _________________________________________________________________________
IMMUNIZATIONS:
Tetanus/Diphtheria (every 10 years):______/_____/______ |
Type administered: _________________________ |
|
Hepatitis B: #1 ____/_____/____ |
#2 _____/____/________ |
#3 _____/_____/______ |
Influenza (Flu):_____/_____/_____ |
|
|
Pneumovax: _____/_____/_____ |
|
|
Other: (specify)__________________________________________ |
|
|
TUBERCULOSIS (TB) SCREENING: (every 2 years by Mantoux method; if positive initial chest |
||
Date given __________ |
Date read___________ |
Results_____________________________________ |
Chest |
Results________________________________________________________ |
|
Is the person free of communicable diseases? Yes No (If no, list specific precautions to prevent the spread of disease to others)
_________________________________________________________________________________________________________
OTHER MEDICAL/LAB/DIAGNOSTIC TESTS:
GYN exam w/PAP: |
Date_____________ |
Results_________________________________________________ |
(women over age 18) |
|
|
Mammogram: |
Date: _____________ |
Results: ________________________________________________ |
(every 2 years- women ages
Prostate Exam: |
Date: _____________ |
Results:______________________________________________________ |
|
(digital |
|
|
|
Hemoccult |
Date: _____________ |
Results:______________________________________________________ |
|
Urinalysis |
Date:______________ |
Results: _________________________________________________ |
|
CBC/Differential |
Date:______________ |
Results: ______________________________________________________ |
|
Hepatitis B Screening |
Date:______________ |
Results: ______________________________________________________ |
|
PSA |
Date:______________ |
Results: ______________________________________________________ |
|
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
HOSPITALIZATIONS/SURGICAL PROCEDURES:
Date
Reason
Date
Reason
12/11/09, revised 7/24/12

PART TWO: GENERAL PHYSICAL EXAMINATION
|
|
|
|
|
Please complete all information to avoid return visits. |
|
|
|
|
|
Blood Pressure:______ /_______ Pulse:_________ |
Respirations:_________ Temp:_________ Height:_________ |
Weight:_________ |
||||
|
|
EVALUATION OF SYSTEMS |
|
|
|
|
||
|
|
|
|
|
|
|
||
|
|
System Name |
|
Normal Findings? |
Comments/Description |
|
||
|
|
Eyes |
|
Yes |
No |
|
|
|
|
|
Ears |
|
Yes |
No |
|
|
|
|
|
Nose |
|
Yes |
No |
|
|
|
|
|
Mouth/Throat |
|
Yes |
No |
|
|
|
|
|
Head/Face/Neck |
|
Yes |
No |
|
|
|
|
|
Breasts |
|
Yes |
No |
|
|
|
|
|
Lungs |
|
Yes |
No |
|
|
|
|
|
Cardiovascular |
|
Yes |
No |
|
|
|
|
|
Extremities |
|
Yes |
No |
|
|
|
|
|
Abdomen |
|
Yes |
No |
|
|
|
|
|
Gastrointestinal |
|
Yes |
No |
|
|
|
|
|
Musculoskeletal |
|
Yes |
No |
|
|
|
|
|
Integumentary |
|
Yes |
No |
|
|
|
|
|
Renal/Urinary |
|
Yes |
No |
|
|
|
|
|
Reproductive |
|
Yes |
No |
|
|
|
|
|
Lymphatic |
|
Yes |
No |
|
|
|
|
|
Endocrine |
|
Yes |
No |
|
|
|
|
|
Nervous System |
|
Yes |
No |
|
|
|
|
|
VISION SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
HEARING SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
ADDITIONAL COMMENTS: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Medical history summary reviewed? |
Yes |
No |
|
|
||
Medication added, changed, or deleted: (from this appointment)__________________________________________________________
Special medication considerations or side effects: ________________________________________________________________
Recommendations for health maintenance: (include need for lab work at regular intervals, treatments, therapies, exercise, hygiene, weight control, etc.)
___________________________________________________________________________________________________________
Recommendations for manual breast exam or manual testicular exam: (include who will perform and frequency)____________________
___________________________________________________________________________________________________________
Recommended diet and special instructions: ____________________________________________________________________
Information pertinent to diagnosis and treatment in case of emergency:
___________________________________________________________________________________________________________
Limitations or restrictions for activities (including work day, lifting, standing, and bending): No Yes (specify)
___________________________________________________________________________________________________________ |
|||
Does this person use adaptive equipment? |
No |
Yes (specify):________________________________________________ |
|
Change in health status from previous year? No |
Yes (specify):_________________________________________________ |
||
This individual is recommended for ICF/ID level of care? (see attached explanation) Yes |
No |
||
Specialty consults recommended? No |
Yes (specify):_________________________________________________________ |
||
Seizure Disorder present? No Yes (specify type):__________________________________ Date of Last Seizure: ______________ |
|||
________________________________ |
_______________________________ |
_________________ |
|
Name of Physician (please print) |
Physician’s Signature |
|
Date |
Physician Address: _____________________________________________ |
Physician Phone Number: ____________________________ |
||
12/11/09, revised 7/24/12
More About Annual Physical Examination
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form is designed to collect essential health information from individuals prior to their medical appointment. This information helps healthcare providers assess the patient's health status, medical history, and any current medications or conditions. Completing this form accurately can facilitate a more efficient and effective examination process.
What information is required in Part One of the form?
Part One requires personal details such as the individual's name, date of birth, address, and Social Security Number. It also asks for the name of any accompanying person and details about significant health conditions, current medications, allergies, and immunizations. This section aims to provide healthcare providers with a comprehensive overview of the individual's health background.
How should current medications be documented?
Current medications should be listed in a structured format that includes the medication name, dosage, frequency, diagnosis, prescribing physician, and the date the medication was prescribed. If additional space is needed, individuals may attach a second page. It is important to indicate whether the person takes medications independently.
What is the significance of the Tuberculosis (TB) screening section?
The Tuberculosis screening section is crucial for identifying potential TB infections. It requires the date the TB test was administered, the date it was read, and the results. If the test is positive, a chest x-ray is typically recommended. This information helps ensure that communicable diseases are managed appropriately to protect both the individual and the community.
What should be included in the evaluation of systems?
The evaluation of systems section requires the assessment of various bodily systems, including eyes, ears, nose, and others. For each system, the healthcare provider will indicate whether normal findings were observed. Any comments or descriptions of abnormal findings should also be noted. This evaluation aids in identifying any health issues that may require further attention.
What recommendations may be provided after the examination?
After the examination, healthcare providers may offer recommendations for health maintenance, which can include suggestions for lab work, treatments, therapies, exercise, and dietary changes. They may also advise on limitations for activities and the need for specialist referrals. These recommendations are tailored to the individual’s health status and needs.
How can individuals ensure their form is completed correctly?
To ensure the form is completed correctly, individuals should take their time to fill out all sections thoroughly and accurately. It is beneficial to gather relevant health information, such as a list of current medications and any previous medical records, before filling out the form. If there are any uncertainties, individuals should feel encouraged to ask for assistance from healthcare staff.
Key takeaways
Filling out the Annual Physical Examination form is an important step in maintaining health. Here are some key takeaways to consider:
- Complete All Sections: Ensure every part of the form is filled out completely. Incomplete forms may lead to additional visits.
- Accurate Personal Information: Provide correct personal details, including your name, address, and date of birth. This helps in identifying your records accurately.
- Medication List: Include a comprehensive list of current medications. If necessary, attach an additional page for detailed information.
- Health History: Document any significant health conditions and past medical history. This information is crucial for your healthcare provider.
- Immunization Records: Keep track of immunizations received. This includes dates and types of vaccines, which are vital for preventive care.
- Communicable Diseases: Indicate if you are free from communicable diseases. If not, specify precautions to prevent spreading illness.
- System Evaluations: Answer questions regarding normal findings for various body systems. This helps your physician assess your overall health.
- Recommendations: Pay attention to any recommendations for health maintenance provided by your physician. Follow these suggestions for better health outcomes.
- Sign and Date: Don’t forget to sign and date the form. This confirms that the information provided is accurate and complete.
By following these guidelines, you can ensure that your Annual Physical Examination form is filled out correctly, facilitating a smoother and more effective medical appointment.
Form Attributes
| Fact Name | Description |
|---|---|
| Purpose of the Form | The Annual Physical Examination Form is designed to collect essential health information before a medical appointment. |
| Completion Requirement | All sections of the form must be completed to avoid the need for return visits. |
| Patient Information | Key details like name, date of birth, and address are required for accurate identification and medical record keeping. |
| Medication Disclosure | Patients must list current medications, including dosage and prescribing physician, to ensure safe and effective care. |
| Immunization Records | Documentation of immunizations, such as Tetanus and Hepatitis B, is necessary for preventive health measures. |
| TB Screening | TB screening is mandated every two years, using the Mantoux method, to identify potential infections. |
| Health History | A summary of past medical history, including any chronic conditions, is crucial for comprehensive evaluation. |
| Physical Examination | A thorough physical exam is conducted, assessing various systems of the body to identify any health concerns. |
| Legal Requirements | In many states, the completion of this form aligns with healthcare regulations that mandate patient health assessments. |
Other PDF Forms
Odometer Disclosure Texas - The Texas Odometer Statement helps protect buyers from odometer fraud.
Fill Out Pdf on Phone - This form serves as a comprehensive snapshot of your professional life.
In addition to being crucial for the transaction, a Georgia Motorcycle Bill of Sale can often be obtained through various online resources, such as OnlineLawDocs.com, which provides templates and further information on how to ensure your sale is documented correctly.
Printable Direction of Payment Form - Essential for tracking repairs paid by insurance funds.
Dos and Don'ts
Filling out the Annual Physical Examination form accurately is crucial for ensuring a smooth and efficient medical appointment. Here are ten essential dos and don'ts to keep in mind:
- Do fill out all personal information completely, including your name, address, and date of birth.
- Don't leave any sections blank. Incomplete forms may lead to delays or the need for return visits.
- Do list all current medications, including dosage and frequency. This helps your physician understand your health better.
- Don't forget to mention any allergies or sensitivities. This information is vital for your safety.
- Do provide details about any significant health conditions or medical history. Transparency is key to effective treatment.
- Don't skip the immunization section. Accurate records can prevent unnecessary vaccinations.
- Do double-check the dates of any previous tests or procedures listed. Accurate timelines are important for your care.
- Don't ignore the evaluation of systems section. This helps identify any potential issues that may need further attention.
- Do ensure that your physician’s signature and contact information are included at the end of the form.
- Don't hesitate to ask for help if you're unsure about any part of the form. It's better to ask than to guess.