Advance Beneficiary Notice of Non-coverage PDF Form
The Advance Beneficiary Notice of Non-coverage (ABN) form plays a crucial role in the healthcare landscape, particularly for Medicare beneficiaries. This form is issued by healthcare providers when they believe that a service or item may not be covered by Medicare. By using the ABN, providers inform patients about the potential financial implications of receiving certain services, allowing beneficiaries to make informed decisions about their care. The form outlines the specific service in question, explains why it may not be covered, and provides patients with options regarding their care. Patients are given the opportunity to either accept responsibility for payment if the service is not covered or decline the service altogether. Understanding the ABN is essential for beneficiaries to navigate their healthcare options effectively and to avoid unexpected costs. This notice not only enhances transparency between patients and providers but also empowers individuals to take control of their healthcare choices.
Common mistakes
-
Neglecting to read the instructions carefully. Many individuals rush through the form without fully understanding the guidelines, leading to errors.
-
Failing to provide accurate personal information. Incomplete or incorrect details can delay processing and cause confusion.
-
Not checking the dates. Ensure that the dates of service are accurate. Mistakes here can affect coverage determinations.
-
Ignoring the reason for non-coverage. Clearly stating the reasons for non-coverage is essential. Omitting this can result in misunderstandings.
-
Overlooking signatures. Both the beneficiary and the provider must sign the form. Missing signatures can invalidate the document.
-
Not keeping a copy. Failing to retain a copy of the completed form for personal records can lead to issues later on.
-
Misunderstanding the implications. Some individuals do not fully grasp what signing the form means for their financial responsibility.
-
Submitting the form without a review. Rushing to submit without double-checking for errors can lead to complications.
-
Assuming the form is unnecessary. Some people mistakenly believe they do not need to fill out the form, which can lead to unexpected costs.
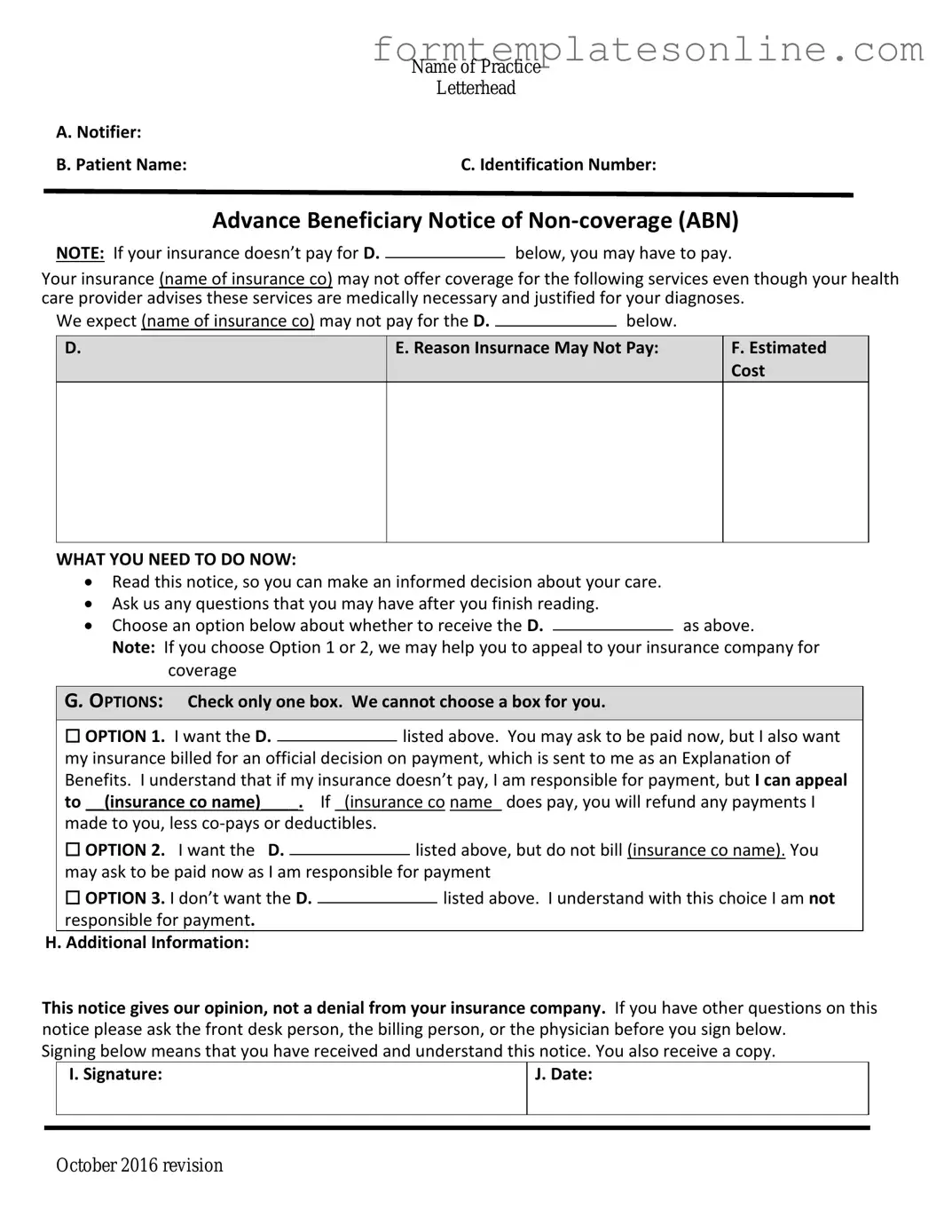
Example - Advance Beneficiary Notice of Non-coverage Form
|
Name of Practice |
|
Letterhead |
A. Notifier: |
|
B. Patient Name: |
C. Identification Number: |
Advance Beneficiary Notice of
NOTE: If your insurance doesn’t pay for D.below, you may have to pay.
Your insurance (name of insurance co) may not offer coverage for the following services even though your health care provider advises these services are medically necessary and justified for your diagnoses.
We expect (name of insurance co) may not pay for the D. |
|
below. |
|
D.
E. Reason Insurnace May Not Pay:
F.Estimated Cost
WHAT YOU NEED TO DO NOW:
Read this notice, so you can make an informed decision about your care.
Ask us any questions that you may have after you finish reading.
Choose an option below about whether to receive the D.as above.
Note: If you choose Option 1 or 2, we may help you to appeal to your insurance company for coverage
G. OPTIONS: Check only one box. We cannot choose a box for you.
|
☐ OPTION 1. I want the D. |
|
listed above. You may ask to be paid now, but I also want |
||||
|
|
||||||
|
my insurance billed for an official decision on payment, which is sent to me as an Explanation of |
||||||
|
Benefits. I understand that if my insurance doesn’t pay, I am responsible for payment, but I can appeal |
||||||
|
to __(insurance co name)____. If _(insurance co name_ does pay, you will refund any payments I |
||||||
|
made to you, less |
|
|
|
|||
|
☐ OPTION 2. I want the D. |
|
|
listed above, but do not bill (insurance co name). You |
|||
|
|
|
|||||
|
may ask to be paid now as I am responsible for payment |
||||||
|
☐ OPTION 3. I don’t want the D. |
|
|
|
listed above. I understand with this choice I am not |
||
|
|
|
|
||||
|
responsible for payment. |
|
|
|
|||
H. Additional Information: |
|
|
|
||||
This notice gives our opinion, not a denial from your insurance company. If you have other questions on this notice please ask the front desk person, the billing person, or the physician before you sign below.
Signing below means that you have received and understand this notice. You also receive a copy.
|
I. Signature: |
J. Date: |
|
|
|
|
|
|
October 2016 revision
More About Advance Beneficiary Notice of Non-coverage
What is the Advance Beneficiary Notice of Non-coverage (ABN)?
The Advance Beneficiary Notice of Non-coverage, commonly known as the ABN, is a form that healthcare providers give to Medicare beneficiaries. It informs patients that Medicare may not cover a specific service or item. By signing the ABN, patients acknowledge they understand the potential for non-coverage and agree to pay for the service if Medicare denies it.
When should I receive an ABN?
You should receive an ABN before receiving a service or item that your provider believes may not be covered by Medicare. This typically happens when the provider thinks that the service is not medically necessary or if it falls outside of Medicare's coverage guidelines.
Do I have to sign the ABN?
Signing the ABN is not mandatory, but it is highly recommended. By signing, you acknowledge that you understand the potential for non-coverage and agree to take financial responsibility if Medicare denies payment. If you choose not to sign, your provider may not perform the service, as they may not be willing to take the risk of non-payment.
What happens if I don’t sign the ABN?
If you do not sign the ABN, your provider may decide not to provide the service. This is because they want to avoid the risk of not getting paid. However, if you do receive the service without signing the ABN, Medicare may deny payment, leaving you responsible for the full cost.
Can I appeal if Medicare denies payment after I signed the ABN?
Yes, you can appeal Medicare's denial of payment even after signing the ABN. The appeal process allows you to present your case, and there may be circumstances under which Medicare will reconsider its decision. Make sure to keep copies of all documents related to your case, including the signed ABN.
What if I receive an ABN but still believe the service should be covered?
If you receive an ABN but believe the service should be covered by Medicare, you have the right to proceed with the service and then appeal the denial if it occurs. It’s important to communicate with your healthcare provider about your concerns and ensure that you understand the reasons for the ABN.
Is there a time limit for appealing a Medicare denial?
Yes, there are time limits for appealing a Medicare denial. Generally, you have 120 days from the date of the denial to file your appeal. It’s crucial to act quickly and follow the specific instructions provided in the denial notice to ensure your appeal is considered.
What should I do if I have questions about the ABN?
If you have questions about the ABN or the services it pertains to, don’t hesitate to reach out to your healthcare provider. They can provide clarification on why the ABN was issued and what it means for your specific situation. Additionally, you can contact Medicare directly for further assistance.
Can I request an ABN for any service?
While you can request an ABN for any service, it is ultimately up to the healthcare provider to decide whether to issue one. Providers typically issue ABNs for services they believe may not be covered by Medicare. If you feel uncertain about a service, it’s always best to ask your provider about the possibility of receiving an ABN.
What should I do if I receive a bill after signing the ABN?
If you receive a bill after signing the ABN, it indicates that Medicare has denied coverage for the service. Review the bill carefully and ensure it matches the services you received. If you believe the charge is incorrect or if you have questions, contact your provider's billing department for clarification and guidance on the next steps.
Key takeaways
The Advance Beneficiary Notice of Non-coverage (ABN) form is an important document for Medicare beneficiaries. Here are key takeaways to understand its purpose and usage:
- The ABN informs patients that a specific service may not be covered by Medicare, allowing them to make informed decisions about their healthcare.
- Patients should receive the ABN before the service is provided, ensuring they understand their potential financial responsibility.
- It is crucial to fill out the form accurately, specifying the service in question and the reason for the non-coverage notice.
- Beneficiaries have the right to refuse the service after receiving an ABN, but they should be aware of the financial implications.
- Keep a copy of the signed ABN for personal records, as it may be necessary for future reference or disputes.
- Understanding the ABN can help beneficiaries appeal any unexpected charges or denials from Medicare.
Form Attributes
| Fact Name | Details |
|---|---|
| Purpose | The Advance Beneficiary Notice of Non-coverage (ABN) informs patients that a service may not be covered by Medicare. |
| When to Use | Providers use the ABN when they believe Medicare might deny payment for a service or item. |
| Patient Rights | Patients have the right to refuse services after receiving an ABN and understanding the potential costs. |
| Signature Requirement | Patients must sign the ABN to acknowledge they understand the potential non-coverage. |
| State-Specific Forms | Some states may have additional requirements or specific forms based on state laws. |
| Governing Law | In California, for example, the ABN is governed by the California Code of Regulations, Title 22. |
| Timing | The ABN should be given to the patient before the service is provided to ensure informed consent. |
| Impact on Billing | If a patient signs an ABN and the service is denied, the provider can bill the patient directly for the service. |
Other PDF Forms
Gift Coupon Template - The recipient can use this gift towards their favorite item or service.
This Independent Contractor Agreement is a vital resource for understanding your rights and responsibilities in contractual relationships, helping you navigate the complexities of agreements in Florida. For more information on this form, consider our overview of the essential Independent Contractor Agreement considerations.
How to Fill Out Disability Forms - Make sure to keep a copy of the completed DE 2501 for your records.
Fill Out Pdf on Phone - The information you provide is confidential and will be protected.
Dos and Don'ts
When filling out the Advance Beneficiary Notice of Non-coverage (ABN) form, it's important to ensure accuracy and clarity. Here are some key do's and don'ts to keep in mind:
- Do read the entire form carefully before filling it out.
- Do provide all necessary information, including your name, Medicare number, and the service being provided.
- Do ask questions if you are unsure about any part of the form.
- Do keep a copy of the completed form for your records.
- Don't leave any required fields blank; this could delay processing.
- Don't use unclear or ambiguous language when describing the service.
- Don't sign the form until you fully understand what you are agreeing to.
- Don't forget to submit the form in a timely manner to avoid coverage issues.